Validity and Reliability of Iraqi Anti-Diabetic Medication Adherence Scale (IADMAS) in Type 1 Diabetic Patients
DOI:
https://doi.org/10.54133/ajms.v9i2.2390Keywords:
IADMAS, Iraq, Reliability, Type 1 diabetes, ValidityAbstract
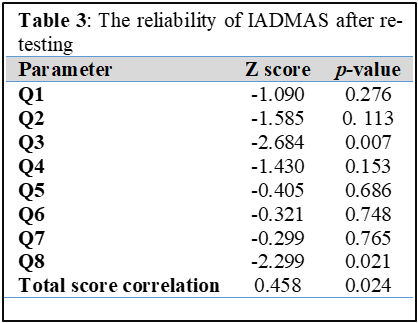
Background: Assessing medication adherence is crucial for patients with type 1 diabetes (T1DM), as it is a primary obstacle to achieving optimal glycemic control in this population. However, none of the currently available tools to assess medication adherence are specific to Iraqi patients with T1DM. Objective: To assess the reliability and validity of the Iraqi Anti-Diabetic Medication Adherence Scale (IADMAS) among Iraqi patients with T1DM. Methods: This cross-sectional study was conducted from January 29 to May 29, 2025, at the Faiha Specialized Diabetes, Endocrine, and Metabolism Center in Basrah, Iraq. It involved 100 Iraqi T1D patients aged≥12 years diagnosed for at least 12 months and on stable treatment for at least 3 months. Participants completed a paper-based IADMAS questionnaire at baseline. Reliability was assessed using Cronbach’s alpha. For test-retest reliability, 24 participants completed the questionnaire again after two weeks, and their scores were correlated using Spearman’s rho. Concurrent validity was examined by comparing IADMAS scores with HbA1c levels. Results: The internal consistency of IADMAS, assessed using Cronbach's alpha (0.217). It can be slightly elevated to 0.266 if item 4 is removed. Regarding the test-retest results, the correlation for the total IADMAS scores was 0.458(p=0.024). By inspecting individual items within IADMAS, two items showed significant differences between test and retest values. There was a non-significant association between IADMAS score and HbA1c (Spearman's ρ = −0.087, p=0.391). Conclusions: IADMAS has poor validity and reliability and hence it is not suitable to assess medication adherence among T1DM patients.
Downloads
References
Kim NH. Diabetes mellitus, still major threat to mortality from various causes. Diabetes Metab J. 2019;43(3):273-275. doi: 10.4093/dmj.2018.0102. DOI: https://doi.org/10.4093/dmj.2018.0102
Campos C. Chronic Hyperglycemia and glucose toxicity: Pathology and clinical sequelae. Postgrad Med. 2012;124(6):90–97. doi: 10.3810/pgm.2012.11.2615. DOI: https://doi.org/10.3810/pgm.2012.11.2615
Mikhael EM, Hassali MA, Hussain SA. Need of self-management education for Iraqi diabetic patients. J Soc Health Diabetes. 2020;8(01):001-2. doi: 10.1055/s-0040-1715994. DOI: https://doi.org/10.1055/s-0040-1715994
Azar S, MarounAbouJaoude N, Kędzia A, Niechciał E. Barriers to type 1 diabetes adherence in adolescents. J Clin Med. 2024;13(19):5669. doi: 10.3390/jcm13195669. DOI: https://doi.org/10.3390/jcm13195669
Boonpattharatthiti K, Saensook T, Neelapaijit N, Sakunrag I, Krass I, Dhippayom T. The prevalence of adherence to insulin therapy in patients with diabetes: A systematic review and meta-analysis. Res Soc Adm Pharm. 2024;20(3):255-295. doi: 10.1016/j.sapharm.2023.11.009. DOI: https://doi.org/10.1016/j.sapharm.2023.11.009
Jabbar RK, Jammal MY. Factors associated with adherence to insulin self-administration among children and adolescents with type 1 DM in Iraq. Iraqi J Pharm Sci. 2023; 32(Suppl.):291-299. doi: 10.31351/vol32issSuppl.pp291-299. DOI: https://doi.org/10.31351/vol32issSuppl.pp291-299
Culig J, Leppee M. From Morisky to Hill-bone; self-reports scales for measuring adherence to medication. Colleg Antropol. 2014;38(1):55-62.
Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015(1):217047. doi: 10.1155/2015/217047. DOI: https://doi.org/10.1155/2015/217047
Chia LR, Schlenk EA, Dunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs Aging. 2006;23(3):191-202. doi: 10.2165/00002512-200623030-00002. DOI: https://doi.org/10.2165/00002512-200623030-00002
Mikhael EM, Hussain SA, Shawky N, Hassali MA. Validity and reliability of anti-diabetic medication adherence scale among patients with diabetes in Baghdad, Iraq: a pilot study. BMJ Open Diabetes Res Care. 2019;7(1). doi: 10.1136/bmjdrc-2019-000658. DOI: https://doi.org/10.1136/bmjdrc-2019-000658
Gan MJ, Albanese-O’Neill A, Haller MJ. Type 1 diabetes: current concepts in epidemiology, pathophysiology, clinical care, and research. Curr Probl Pediatr Adolesc Health Care. 2012;42(10):269-291. doi: 10.1016/j.cppeds.2012.07.002. DOI: https://doi.org/10.1016/j.cppeds.2012.07.002
American Diabetes Association Professional Practice Committee; 5. Facilitating positive health behaviors and well-being to improve health outcomes: Standards of care in diabetes—2025. Diabetes Care. 2025;48 (Supplement_1): S86–S127. doi: 10.2337/dc25-S005. DOI: https://doi.org/10.2337/dc25-S005
Hatun Ş, Gökçe T, Can E, Eviz E, Karakuş KE, Smart C, et al. Current management of type 1 diabetes in children: Guideline-based expert opinions and recommendations. J Clin Res Pediatr Endocrinol. 2024. doi: 10.4274/jcrpe.galenos.2024.2024-1-15. DOI: https://doi.org/10.4274/jcrpe.galenos.2024.2024-1-15
Małachowska M, Gosławska Z, Rusak E, Jarosz-Chobot P. The role and need for psychological support in the treatment of adolescents and young people suffering from type 1 diabetes. Front. Psychol. 2023;13:945042. doi: 10.3389/fpsyg.2022.945042. DOI: https://doi.org/10.3389/fpsyg.2022.945042
Nunnally JC, Bernstein IH. Psychometric Theory, McGraw-Hill. New York. 1994;136.
Memon MA, Ting H, Cheah JH, Thurasamy R, Chuah F, Cham TH. Sample size for survey research: Review and recommendations. JASEM. 2020;4(2):i-xx. doi: 10.47263/jasem.4(2)01. DOI: https://doi.org/10.47263/JASEM.4(2)01
Mikhael EM, Hassali MA, Hussain SA. Clinical trials among Arab diabetic patients; the challenges. Diabetes Metab Syndr. 2019;14(1):1. doi: 10.1016/j.dsx.2019.11.011. DOI: https://doi.org/10.1016/j.dsx.2019.11.011
Izah SC, Sylva L, Hait M. Cronbach's alpha: A cornerstone in ensuring reliability and validity in environmental health assessment. ES Energy Environment. 2023;23:1057. doi: 10.30919/esee1057. DOI: https://doi.org/10.30919/esee1057
Hajjar S. Statistical analysis: internal-consistency reliability and construct validity. Int J Quan. Qualit Res Meth. 2018;6(1):46–57.
Raharjanti NW, Wiguna T, Purwadianto A, Soemantri D, Indriatmi W, Poerwandari EK, et al. Translation, validity and reliability of decision style scale in forensic psychiatric setting in Indonesia. Heliyon. 2022;8(7):e09810. doi: 10.1016/j.heliyon.2022.e09810. DOI: https://doi.org/10.1016/j.heliyon.2022.e09810
Evans JD. Straightforward statistics for the behavioral sciences. Thomson Brooks/Cole Publishing Co; 1996.
Abd-Alrahman MS, Jasim AL, Alhilal MA. Enhancing adherence and satisfaction with insulin therapy in type 1 diabetes mellitus patients through pharmacist-led interventions: Interventional study. Bahrain Med Bull. 2025 Jun; 47(2):2195.
Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Ed. 2018;48(6):1273-1296. doi 10.1007/s11165-016-9602-2. DOI: https://doi.org/10.1007/s11165-016-9602-2
Osburn HG. Coefficient alpha and related internal consistency reliability coefficients. Psychol Methods. 2000;5(3):343-355. doi: 10.1037/1082-989x.5.3.343. DOI: https://doi.org/10.1037//1082-989X.5.3.343
Almahfoodh D, Alabbood M, Alali A, Mansour A. Epidemiology of type 1 diabetes mellitus in Basrah, Southern Iraq: A retrospective study. Diabetes Res Clin Pract. 2017;133:104-108. doi: 10.1016/j.diabres.2017.09.001. DOI: https://doi.org/10.1016/j.diabres.2017.09.001
Moon SJ, Lee WY, Hwang JS, Hong YP, Morisky DE. Accuracy of a screening tool for medication adherence: A systematic review and meta-analysis of the Morisky Medication Adherence Scale-8. PLoS One. 2017;12(11):e0187139. doi: 10.1371/journal.pone.0187139. DOI: https://doi.org/10.1371/journal.pone.0187139
de Torres-Sánchez A, Ampudia-Blasco FJ, Murillo S, Bellido V, Amor AJ, Mezquita-Raya P. Proposed practical guidelines to improve glycemic management by reducing glycemic variability in people with type 1 diabetes mellitus. Diabetes Ther. 2025:1-21. doi: 10.1007/s13300-025-01703-0. DOI: https://doi.org/10.1007/s13300-025-01703-0
Talabani SN, Mikhael EM. Exploring adherence, treatment experiences, and quality of healthcare services in HIV management among Iraqi patients: Challenges and influential factors. HIV AIDS (Auckl). 2025;17:227-240. doi: 10.2147/HIV.S539087. DOI: https://doi.org/10.2147/HIV.S539087
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).