Dexamethasone versus Fentanyl as Adjuvants to Intrathecal Bupivacaine Anesthesia in Cesarean Section: Impacts on Analgesia Duration and Postoperative Outcomes
DOI:
https://doi.org/10.54133/ajms.v9i2.2350الكلمات المفتاحية:
Analgesia، Bupivacaine، Cesarean section، Dexamethasone، Fentanylالملخص
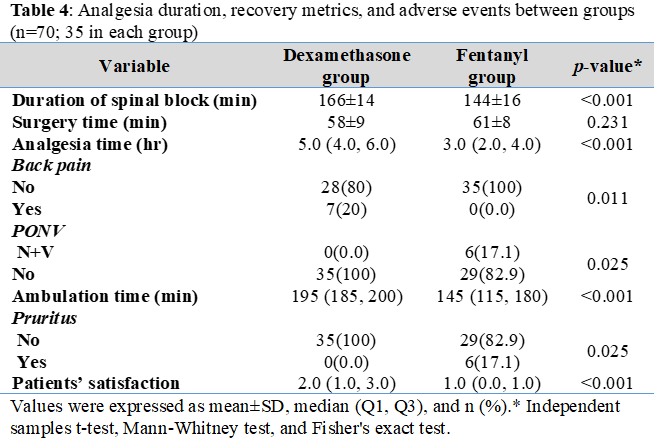
Background: Effective postoperative analgesia after cesarean section is essential to facilitate early maternal recovery and reduce opioid-related side effects. Although fentanyl is commonly used as an intrathecal adjuvant to bupivacaine, concerns about adverse effects such as pruritus and nausea have prompted exploration of alternatives like dexamethasone. Objective: To compare the efficacy and safety of intrathecal dexamethasone versus fentanyl as adjuvants to 0.5% bupivacaine in spinal anesthesia for cesarean section. Methods: In this quasi-randomized clinical study, 70 women undergoing elective cesarean section were allocated to receive spinal anesthesia with bupivacaine plus either fentanyl (10–25µg; Group F) or dexamethasone (2–4mg; Group D). Hemodynamic parameters, duration of postoperative analgesia, incidence of side effects, ambulation time, and patient satisfaction were assessed using validated instruments. Results: Group D demonstrated significantly longer analgesia duration (median 5.0 h [IQR 4.0–6.0]) compared to Group F (3.0 h [IQR 2.0–4.0], p<0.001). Post-spinal systolic blood pressure and heart rate were significantly higher in the dexamethasone group but remained within physiological limits. Adverse events such as pruritus and postoperative nausea/vomiting were significantly more frequent in Group F, while back pain was reported only in Group D (20%, p=0.011). Patient satisfaction was higher in group F (p<0.001), potentially due to earlier ambulation. Conclusions: Intrathecal dexamethasone is a safe and effective adjuvant to bupivacaine in cesarean section spinal anesthesia, offering prolonged analgesia and fewer opioid-related side effects compared to fentanyl. Further randomized trials with longer follow-up and neonatal outcomes are warranted.
التنزيلات
المراجع
Pan PH. Post cesarean delivery pain management: multimodal approach. Int J Obstet Anesthesia. 2006;15(3):185-188. doi: 10.1016/j.ijoa.2006.04.004. DOI: https://doi.org/10.1016/j.ijoa.2006.04.004
Elfarargy MS, Ahmad AR, Elbadry DH. Neonatal pain management: Is there an endocrinal response? Endocr Metab Immune Disord Drug Targets. 2025. doi: 10.2174/0118715303325556241127080237. DOI: https://doi.org/10.2174/0118715303325556241127080237
Nasr IA, Elokda SA. Safety and efficacy of intrathecal adjuvants for cesarean section: bupivacaine, sufentanil, or dexmedetomidine. Ain Shams J Anesthesiol. 2015;8(3). DOI: https://doi.org/10.4103/1687-7934.159002
Cooper DW, Turner G. Patient-controlled extradural analgesia to compare bupivacaine, fentanyl and bupivacaine with fentanyl in the treatment of postoperative pain. Br J Anaesth. 1993;70(5):503-507. doi: 10.1093/bja/70.5.503. DOI: https://doi.org/10.1093/bja/70.5.503
Paul AK, Smith CM, Rahmatullah M, Nissapatorn V, Wilairatana P, Spetea M, et al. Opioid analgesia and opioid-induced adverse effects: A review. Pharmaceuticals (Basel). 2021;14(11):1091. doi: 10.3390/ph14111091. DOI: https://doi.org/10.3390/ph14111091
Desai N, Kirkham KR, Albrecht E. Local anaesthetic adjuncts for peripheral regional anaesthesia: a narrative review. Anaesthesia. 2021;76 Suppl 1:100-109. doi: 10.1111/anae.15245. DOI: https://doi.org/10.1111/anae.15245
Abebe M, Alemu B, Teku G, Eshetu O, Wale E, Besha A, et al. Effectiveness of single intravenous dexamethasone in prolongation of spinal anesthesia for postoperative analgesia in elective cesarean section: A systematic review of randomized controlled trials. J Pain Res. 2024;17:1361-1368. doi: 10.2147/JPR.S451595. DOI: https://doi.org/10.2147/JPR.S451595
Jagdale S, Kakade AS, Wagh G: Comparison of the efficacy of bupivacaine versus bupivacaine plus dexamethasone during surgical TAP block for post operative analgesia after caesarean section. Indian J Obstet Gynecol Res. 2019;6(4):492-494. doi: 10.18231/j.ijogr.2019.106. DOI: https://doi.org/10.18231/j.ijogr.2019.106
Khafagy HF, Refaat AI, El-Sabae HH, Youssif MA. Efficacy of epidural dexamethasone versus fentanyl on postoperative analgesia. J Anesth. 2010;24(4):531-536. doi: 10.1007/s00540-010-0949-7. DOI: https://doi.org/10.1007/s00540-010-0949-7
Uppal V, Retter S, Casey M, Sancheti S, Matheson K, McKeen DM. Efficacy of intrathecal fentanyl for cesarean delivery: A systematic review and meta-analysis of randomized controlled trials with trial sequential analysis. Anesth Analg. 2020;130(1):111-125. doi: 10.1213/ANE.0000000000003975. DOI: https://doi.org/10.1213/ANE.0000000000003975
Li Z, Tian M, Zhang CY, Li AZ, Huang AJ, Shi CX, et al. A randomised controlled trial to evaluate the effectiveness of intrathecal bupivacaine combined with different adjuvants (fentanyl, clonidine and dexmedetomidine) in caesarean section. Drug Res (Stuttg). 2015;65(11):581-586. doi: 10.1055/s-0034-1395614. DOI: https://doi.org/10.1055/s-0034-1395614
Ali MA, Ismail S, Sohaib M, Aman A. A double-blind randomized control trial to compare the effect of varying doses of intrathecal fentanyl on clinical efficacy and side effects in parturients undergoing cesarean section. J Anaesthesiol Clin Pharmacol. 2018;34(2):221-226. doi: 10.4103/joacp.JOACP_271_16. DOI: https://doi.org/10.4103/joacp.JOACP_271_16
Tantry TP, Shetty V, Deepak A, Murali S, Golitadka MSB, Menon SK, et al. Efficacy and safety of adjuvant intrathecal dexamethasone during spinal anesthesia: A systematic review and meta-analysis. Saudi J Anaesth. 2024;18(3):417-428. doi: 10.4103/sja.sja_112_24. DOI: https://doi.org/10.4103/sja.sja_112_24
Mohamed RT, Hammad RA, Kamar NM, Mohamed MM. Intravenous dexamethasone versus intrathecal dexamethasone in prolonging the duration of spinal anesthesia and postoperative analgesia in elective cesarean section. QJM Inte J Med. 2024;117(Supplement_1):hcae070. 030. doi: 10.1093/qjmed/hcae070.030. DOI: https://doi.org/10.1093/qjmed/hcae070.030
Fetene MB, Bayable SD, Wendimu ES, Belehu KD, Almaw AA, Dula PK, et al. Perioperative patient satisfaction and its predictors following surgery and anesthesia services in North Shewa, Ethiopia. A multicenter prospective cross-sectional study. Ann Med Surg. 2022;76:103478. doi: 10.1016/j.amsu.2022.103478. DOI: https://doi.org/10.1016/j.amsu.2022.103478
Nasiri A, Abutorabi SM, Sane S. Intrathecal dexamethasone-bupivacaine combination with bupivacaine alone in spinal anesthesia for cesarean delivery. Caspian J Intern Med. 2024;15(3):414-420. doi: 10.22088/cjim.15.3.414.
El-Shourbagy MA, Mammdouh AM, Shawky ME, Mohamed HA. Addition of intrathecal dexamethasone to bupivacaine for spinal anesthesia in cesarean section. Evid Based Women's Health J. 2019;9(2):416-424. doi: 10.21608/ebwhj.2019.33474. DOI: https://doi.org/10.21608/ebwhj.2019.33474
Ahmed SA, Lotfy HA, Mostafa TAH. The effect of adding dexmedetomidine or dexamethasone to bupivacaine-fentanyl mixture in spinal anesthesia for cesarean section. J Anaesthesiol Clin Pharmacol. 2024;40(1):82-89. doi: 10.4103/joacp.joacp_396_22. DOI: https://doi.org/10.4103/joacp.joacp_396_22
Comer SD, Cahill CM. Fentanyl: Receptor pharmacology, abuse potential, and implications for treatment. Neurosci Biobehav Rev. 2019;106:49-57. doi: 10.1016/j.neubiorev.2018.12.005. DOI: https://doi.org/10.1016/j.neubiorev.2018.12.005
Bhuyan S, Chandak AV. Intrathecal fentanyl: A comprehensive review of the pharmacological and clinical profile in anaesthesia. Res J Pharm Technol. 2024;17(6):2959-2966. doi: 10.52711/0974-360X.2024.00463. DOI: https://doi.org/10.52711/0974-360X.2024.00463
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2025 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).