Association Between Non-Alcoholic Fatty Liver Disease and Subclinical Atherosclerosis: A Study of Carotid Intima-Media Thickness
DOI:
https://doi.org/10.54133/ajms.v9i2.2391Keywords:
Body mass index, Carotid intima-media thickness, Fatty liver disease, UltrasoundAbstract
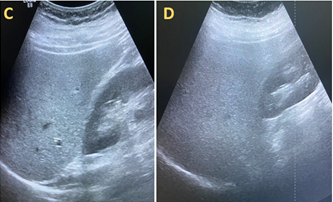
Background: Non-alcoholic fatty liver disease (NAFLD) is a major contributor to chronic liver disease worldwide. It is associated with metabolic syndrome, central obesity, insulin resistance, hypertension, hyperlipidemia, and cardiovascular risks. Carotid intima-media thickness (CIMT) is a recognized surrogate marker for atherosclerosis and cardiovascular risk. Objective: To evaluate the CIMT in patients diagnosed with NAFLD, highlighting potential pathophysiological correlations and clinical implications. Methods: A cross-sectional study was conducted at Al Kindy Teaching Hospital over 4 months from October 2023 to February 2024. The sample size was 100 patients showing ultrasonic signs of fatty liver changes (44 were males and 56 were females). These patients underwent carotid Doppler ultrasound, and the intima-media thickness was measured. Results: Of the 100 patients, 53 had a CIMT greater than 0.08 cm, 23 had grade I fatty liver, 24 had grade II fatty liver, and 6 had grade III fatty liver. Of the 47 patients with a CIMT < 0.08 cm, 16 had grade II fatty liver and 31 had grade I fatty liver. The results were statistically significant (p=0.015). The logistic regression shows a higher fatty liver stage significantly associated with increased IMT, but BMI is not significantly associated with thickened carotid intima-media. Conclusions: NAFLD patients exhibit a higher propensity for subclinical atherosclerosis, as evidenced by increased CIMT, and its monitoring may serve as a valuable noninvasive tool in cardiovascular risk stratification, especially in metabolically compromised NAFLD populations.
Downloads
References
Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021;397(10290):2212-2224. doiI: 10.1016/S0140-6736(20)32511-3. DOI: https://doi.org/10.1016/S0140-6736(20)32511-3
Benedict M, Zhang X. Non-alcoholic fatty liver disease: An expanded review. World J Hepatol. 2017;9(16):715. doi: 10.4254/wjh.v9.i16.715. DOI: https://doi.org/10.4254/wjh.v9.i16.715
Castellanos-Fernández MI, Crespo-Ramírez E, Del Valle-Díaz S, Barreto-Suárez E, Díaz-Elías JO, Corrales-Alonso S, et al. Non-alcoholic fatty liver disease in Cuba. MEDICC Rev. 2021;23(1):64-71. doi: 10.37757/MR2021.V23.N1.11. DOI: https://doi.org/10.37757/MR2021.V23.N1.12
Hassan QA, Abdulqade SK, Bakr GM, A'wad SN, Abdullah RH, Abdalmuhsin HA, et al. Linking NAFLD and nephrolithiasis: A CT-based investigation. J Contemp Med Sci. 2024;10(4). doi: 10.22317/jcms.v10i4.1603. DOI: https://doi.org/10.22317/jcms.v10i4.1603
Savari F, Mard SA. Nonalcoholic steatohepatitis: A comprehensive updated review of risk factors, symptoms, and treatment. Heliyon. 2024;10(7). doi:10.1016/j.heliyon.2024.e28468. DOI: https://doi.org/10.1016/j.heliyon.2024.e28468
Cotter TG, Rinella M. Nonalcoholic fatty liver disease 2020: the state of the disease. Gastroenterology. 2020 May 1;158(7):1851-64. DOI:10.1053/j.gastro.2020.01.052 DOI: https://doi.org/10.1053/j.gastro.2020.01.052
Teng ML, Ng CH, Huang DQ, Chan KE, Tan DJ, Lim WH, et al. Global incidence and prevalence of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2022;29(Suppl):S32. doi: 10.3350/cmh.2022.0365. DOI: https://doi.org/10.3350/cmh.2022.0365
Hamid GR, Khalaf RZ. Association between body mass index and complete blood count Parameters. Int J Stat Med Res. 2025;14:350–354. doi: 10.6000/1929-6029.2025.14.33. DOI: https://doi.org/10.6000/1929-6029.2025.14.33
Juanola O, Martínez-López S, Francés R, Gómez-Hurtado I. Non-alcoholic fatty liver disease: metabolic, genetic, epigenetic and environmental risk factors. Int J Environ Res Public Health. 2021;18(10):5227. doi: 10.3390/ijerph18105227. DOI: https://doi.org/10.3390/ijerph18105227
Nori W, Akram NN, Mueen Al-kaabi M, Al-Ani RM, Pantazi AC. Innovative gut microbiome-targeted strategies: A promising frontier for pediatric inflammatory bowel disease. New Emir Med J. 2024;5(1):e02506882356553. doi: 10.2174/0102506882356553250306050102. DOI: https://doi.org/10.2174/0102506882356553250306050102
Wan Y, Wang D, Li H, Xu Y. The imaging techniques and diagnostic performance of ultrasound, CT, and MRI in detecting liver steatosis and fat quantification: A systematic review. J Radiat Res Appl Sci. 2023;16(4):100658. doi:10.1016/j.jrras.2023.100658. DOI: https://doi.org/10.1016/j.jrras.2023.100658
Ahmed SA, Abdulqader SK, Shakir NA. The efficacy of bedside chest ultrasound in the detection of traumatic pneumothorax. Open Neuroimag J. 2024;17(1). doi: 10.2174/0118744400300817240704095404. DOI: https://doi.org/10.2174/0118744400300817240704095404
Mishra P, Younossi ZM. Abdominal ultrasound for diagnosis of nonalcoholic fatty liver disease (NAFLD). ACG Case Rep J. 2007;102(12):2716-2717. doi: 10.1111/j.1572-0241.2007.01520.x. DOI: https://doi.org/10.1111/j.1572-0241.2007.01520.x
Duell PB, Welty FK, Miller M, Chait A, Hammond G, Ahmad Z, et al. Nonalcoholic fatty liver disease and cardiovascular risk: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2022;42(6):e168-185. doi: 10.1161/ATV.00000000000001. DOI: https://doi.org/10.1161/ATV.0000000000000153
Yang CW, Guo YC, Li CI, Liu CS, Lin CH, Liu CH, et al. Subclinical atherosclerosis markers of carotid intima-media thickness, carotid plaques, carotid stenosis, and mortality in community-dwelling adults. Int J Environ Res Public Health. 2020;17(13):4745. doi: 10.3390/ijerph17134745. DOI: https://doi.org/10.3390/ijerph17134745
Abdulqader S, Bakr GM, Ahmed SA, Hassan QA, Al-Kinani M. Gender distribution of coronary artery calcium score and degree of stenosis assessed by computed tomography angiography in Iraqi patients with chest pain. Al-Rafidain J Med Sci. 2024;7(1):78-84. doi: 10.54133/ajms.v7i1.1032. DOI: https://doi.org/10.54133/ajms.v7i1.1032
Takase M, Nakaya N, Nakamura T, Kogure M, Hatanaka R, Nakaya K, et al. Carotid intima media thickness and risk factor for atherosclerosis: Tohoku medical megabank community-based cohort study. J Atheroscler Thromb. 2023;30(10):1471-1482. doi: 10.5551/jat.64039. DOI: https://doi.org/10.5551/jat.64039
Abosheaishaa H, Nassar M, Abdelhalim O, Bahbah AA, Abbas S, Morsi SM, et al. Relation between non-alcoholic fatty liver disease and carotid artery intimal media thickness as a surrogate for atherosclerosis: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2024;36(5):592-607. doi: 10.1097/MEG.0000000000002721. DOI: https://doi.org/10.1097/MEG.0000000000002721
Seneviratne N, Fang C, Sidhu PS. Ultrasound-based hepatic fat quantification: current status and future directions. Clin Radiol. 2023;78(3):187-200. doi: 10.1016/j.crad.2022.10.003. DOI: https://doi.org/10.1016/j.crad.2022.10.003
Gateva A, Assyov Y, Karamfilova V, Kamenov Z. Common carotid artery intima media thickness (CIMT) in patients with prediabetes and newly diagnosed type 2 diabetes mellitus. J Diabetes Complications. 2024;38(7):108766. doi: 10.1016/j.jdiacomp.2024.108766. DOI: https://doi.org/10.1016/j.jdiacomp.2024.108766
Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6(1):14. PMID: 24834239.
Huang YC, Huang JC, Chien HH, Lin CI, Chuang YS, Cheng HY, et al. Performance of nonalcoholic fatty liver fibrosis score in estimating atherosclerotic cardiovascular disease risk. Nutr Metab Cardiovasc Dis. 2023;33(12):2479-2487. doi: 10.1016/j.numecd.2023.08.005. DOI: https://doi.org/10.1016/j.numecd.2023.08.005
Yoneda M, Yamamoto T, Honda Y, Imajo K, Ogawa Y, Kessoku T, et al. Risk of cardiovascular disease in patients with fatty liver disease as defined from the metabolic dysfunction associated fatty liver disease or nonalcoholic fatty liver disease point of view: a retrospective nationwide claims database study in Japan. J Gastroenterol. 2021;56(11):1022-1032. doi: 10.1007/s00535-021-01828-6. DOI: https://doi.org/10.1007/s00535-021-01828-6
Fernández-Alvarez V, Linares Sánchez M, López Alvarez F, Suárez Nieto C, Mäkitie AA, Olsen KD, et al. Evaluation of intima-media thickness and arterial stiffness as early ultrasound biomarkers of carotid artery atherosclerosis. Cardiol Ther. 2022;11(2):231-247. doi: 10.1007/s40119-022-00261-x. DOI: https://doi.org/10.1007/s40119-022-00261-x
Kawamoto R, Katoh T, Kusunoki T, Ohtsuka N. Carotid atherosclerosis as a surrogate maker of cardiovascular disease in diabetic patients. Int Sch Res Notices. 2013;2013(1):979481. doi: 10.1155/2013/979481. DOI: https://doi.org/10.1155/2013/979481
Veglia F, Malagoni AM, Amato M, Strawbridge RJ, Savonen K, Giral P, et al. Enhancing cardiovascular risk prediction with a simplified carotid IMT protocol: Evidence from the IMPROVE study. Biomedicines. 2025;13(3):584. doi: 10.3390/biomedicines13030584. DOI: https://doi.org/10.3390/biomedicines13030584
Narayan R, Ahmad MS. Carotid intima-media thickness in patients with non-alcoholic fatty liver disease: A study from eastern part of India. Int J Res Med Sci. 2024;12:1640-1646. doi: 10.18203/2320-6012.ijrms20241254. DOI: https://doi.org/10.18203/2320-6012.ijrms20241254
Fotouh AA, Hassaballah MS, Sayed BM. The impact of non-alcoholic fatty liver disease on carotid intima-media thickness: A comprehensive review. Med J Cairo Univ. 2025;93(03):49-55. doi: 10.21608/mjcu.2025.422741. DOI: https://doi.org/10.21608/mjcu.2025.422741
Rasool A, Dar W, Latief M, Dar I, Sofi N, Khan MA. Nonalcoholic fatty liver disease as an independent risk factor for carotid atherosclerosis. Brain Circ. 2017;3(1):35-40. doi: 10.4103/bc.bc_28_16. DOI: https://doi.org/10.4103/bc.bc_28_16
Cai J, Zhang S, Huang W. Association between nonalcoholic fatty liver disease and carotid atherosclerosis: a meta-analysis. Int J Clin Exp Med. 2015;8(5):7673. PMID: 26221316.
Riaz HA, Iqbal J, Arif U. Association between non‐alcoholic fatty liver disease (NAFLD) and raised carotid intima‐media thickness (CIMT). Pak J Med Health Sci. 2016;10:1393-1396. doi: 10.53350/pjmhs221610. DOI: https://doi.org/10.53350/pjmhs221610
Vu H, Tuong TK, Lan NH, Thang TQ, Bilgin K, Hoa T, et al. Association between nonalcoholic fatty liver disease and carotid intima-media thickness. Clin Ter. 2023;174(1). doi: 10.7417/CT.2023.5007.
Khoshbaten M, Maleki SH, Hadad S, Baral A, Rocha AV, Poudel L, et al. Association of nonalcoholic fatty liver disease and carotid media‐intima thickness: A systematic review and a meta‐analysis. Health Sci Rep. 2023;6(9):e1554. doi: 10.1002/hsr2.1554. DOI: https://doi.org/10.1002/hsr2.1554
Tang A, Chen J, Le TA, Changchien C, Hamilton G, Middleton MS, et al. Cross-sectional and longitudinal evaluation of liver volume and total liver fat burden in adults with nonalcoholic steatohepatitis. Abdom Imaging. 2015;40(1):26-37. doi: 10.1007/s00261-014-0175-0. DOI: https://doi.org/10.1007/s00261-014-0175-0
Khanal UP, Paudel B, Gurung G, Hu YS, Kuo CW. Correlational study of nonalcoholic fatty liver disease diagnosed by ultrasonography with lipid profile and body mass index in adult nepalese population. J Med Ultrasound. 2019;27(1):19-25. doi: 10.4103/JMU.JMU_53_18. DOI: https://doi.org/10.4103/JMU.JMU_53_18
Borai IH, Shaker Y, Kamal MM, Ezzat WM, Ashour E, Afify M, et al. Evaluation of biomarkers in Egyptian patients with different grades of nonalcoholic fatty liver disease. J Clin Transl Hepatol. 2017;5(2):109-118. doi: 10.14218/JCTH.2017.00004. DOI: https://doi.org/10.14218/JCTH.2017.00004
Chouhan M, Kansal A, Trikha S, Gupta M. To study the carotid intima media thickness in patients of fatty liver disease. Int J Adv Med. 2017;4:1282-1287. doi: 10.18203/2349-3933.ijam20173715. DOI: 10.14218/JCTH.2017.00004. DOI: https://doi.org/10.18203/2349-3933.ijam20173715
Li A, Yan J, Zhao Y, Yu Z, Tian S, Khan AH, et al. Vascular aging: Assessment and intervention. Clin Interv Aging. 2023;18:1373-1395. doi: 10.2147/CIA.S423373. DOI: https://doi.org/10.2147/CIA.S423373
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 )

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).